The world's leading health organization is sounding serious alarm bells about the problem of antibiotic resistance.
In its first report on the issue ever, the World Health Organization (WHO) is sounding alarms about the issue of antibiotic resistance and the global public health threats it poses to our increasingly interconnected world.
"The problem is so serious that it threatens the achievements of modern medicine. A post-antibiotic era—in which common infections and minor injuries can kill—is a very real possibility for the 21st century," the report states.
Antibiotic resistance occurs when bacteria no longer die when treated with antibiotics. As a result, doctors have to use stronger, more potent antibiotics, and the more those are used, the more resistance bacteria develop to those as well. The WHO is warning that we're reaching a point in which the strongest antibiotics doctors have in their arsenal, the "treatment of last resort" drugs as they're called, no longer work.
And in fact, it's no longer just bacteria that are becoming resistant. The WHO has stopped referring to the problem as "antibiotic resistance" and now calls it "antimicrobial resistance," to encompass other organisms, such as viruses and parasites, that no longer respond to the drugs of choice. Namely, treating the viruses tuberculosis and HIV, and malaria (a parasite), has become harder as these diseases become resistant to medications. Even H1N1, the so-called "swine flu" that reached pandemic levels in 2009, has begun developing resistance to potent antiviral drugs.
Resistance Is a Worldwide Problem
One of the major points of the report is that diseases that used to be restricted to certain locales are now spreading internationally:
Among their key findings:
• Resistance to the treatment of last resort for life-threatening infections caused by a common intestinal bacteria, Klebsiella pneumonia—carbapenem antibiotics—has spread to all regions of the world. K. pneumoniae is a major cause of hospital-acquired infections such as pneumonia, bloodstream infections, infections in newborns and intensive-care unit patients. In some countries, because of resistance, carbapenem antibiotics would not work in more than half of people treated for K. pneumoniae infections.
• Treatment failure to the last resort of treatment for gonorrhea—third generation cephalosporins—has been confirmed in Austria, Australia, Canada, France, Japan, Norway, Slovenia, South Africa, Sweden and the United Kingdom. More than 1 million people are infected with gonorrhoea around the world every day.
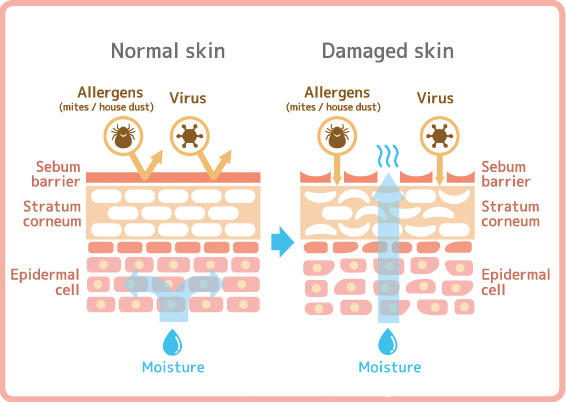
• People with MRSA (methicillin-resistant Staphylococcus aureus) are estimated to be 64 percent more likely to die than people with a non-resistant form of the infection. MRSA, which can cause septic bloodstream infections when exposed to broken skin, is one of the most common "community-acquired" resistant infections, meaning you're likely to pick it up anywhere other people are—your gym, place of worship, a nearby park or even at schools. In the Americas, as many as 90 percent of staph infections are reported to be MRSA.
• There hasn't been a new class of antibiotics developed since the late 1980s.
We Can't Track What We Don't Know
The WHO is calling on countries all over the world to step up their surveillance of these deadly infections, something that happens rarely, if at all. An investigative report, "Hunting the Nightmare Bacteria," that ran on the PBS program Frontline in October 2013 revealed that public health officials in the U.S. have little to no data on the extent of antimicrobial resistance in this country. Healthcare facilities aren't required to report outbreaks, the report found, and many don't because they don't want to scare people or have to deal with bad PR.
“It is frankly embarrassing that we as a country do not know where resistance is occurring, how bad the problem is for various organisms or who’s using what antibiotics when,” Brad Spellberg, MD, an infectious disease doctor at Harbor-UCLA Medical Center, said in the documentary.
The Centers for Disease Control and Prevention has estimated that antimicrobial resistant infections hit two million people a year and kill at least 23,000. But the WHO notes that in most countries around the world, including the U.S., often only the most severe infections are documented and minor community-acquired infections (which can get passed along repeatedly and wind up as a severe infection) go unreported.
Clean Up the Food Supply!
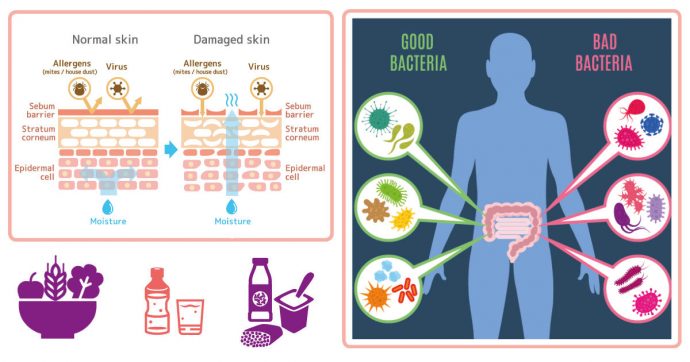
For quite possibly the first time, the WHO also called out the food industry for its contribution to antimicrobial resistance. " The use of antibiotics in animal husbandry—including in livestock, poultry and fish farming—are leading to increasing recognition that urgent action is needed to avoid inappropriate use, and to reduce antibiotic usage in animal husbandry and aquaculture, as well as in humans," the report states. In the U.S., 80 percent of antibiotics sold go into animal feed to prevent infections in healthy animals or to speed growth. And we're not alone. "In many countries, the total amount of antibiotics used in animals (both food-producing and companion animals), measured as gross weight, exceeds the quantity used in the treatment of disease in humans," the authors found.
The same classes of antibiotics used on these animals are the same as those given to humans. In particular, fluoroquinolones, antibiotics used widely in the poultry industry, are increasingly ineffective against urinary tract infections caused by drug-resistant E. coli bacteria, which have been detected on all forms of supermarket meat, and against MRSA soft-tissue and skin infections.
Numerous groups in the U.S. have sued the Food and Drug Administration to revoke its approvals in animals for antibiotics that are valuable for humans. The agency's only response has been to set voluntary guidelines for the industry.
What You Can Do
Despite the damage factory farming has done to antibiotic effectiveness, the WHO and other public health officials insist that the first line of defense in controlling the problem of antimicrobial resistance is the healthcare setting: Stopping doctors from giving patients antibiotics for conditions they aren't designed to treat, for instance, when you're given antibiotics for a cold that's caused by a virus, not bacteria.
• Don't automatically ask for antibiotics when you feel sick and visit a doctor.
• If your doctor prescribes an antibiotic, ask if there's an alternative before just accepting the advice. Some doctors feel compelled to offer the drugs to make people feel better, but asking for an alternative can open up a dialogue about other options.
• When you do need an antibiotic, take the full course, even if you're feeling better.
• Wash your hands frequently to protect yourself from community-acquired infections, and keep your hands away from your nose, eyes and mouth, where infections can enter.
Contributed by By EMILY MAIN
 Alarm bells over antibiotic resistance
The World Health Organisation’s most comprehensive report to date sounds a warning that we are entering a world where antibiotics have little effect.
Alarm bells over antibiotic resistance
The World Health Organisation’s most comprehensive report to date sounds a warning that we are entering a world where antibiotics have little effect.
THE World Health Organisation (WHO) has sounded a warning that many types of disease-causing bacteria can no longer be treated with the usual antibiotics and the benefits of modern medicine are increasingly being eroded.
The comprehensive 232-page report on anti-microbial resistance with data from 114 countries shows how this threat is happening now in every region of the world and can affect anyone in any country.
Antibiotic resistance – when bacteria evolve so that antibiotics no longer work to treat infections – is described by the report as “a problem so serious that it threatens the achievements of modern medicine”.
“A post-antibiotic era, in which common infections and minor injuries can kill, far from being an apocalyptic fantasy, is instead a very real possibility for the 21st century,” said Dr Keiji Fukuda, WHO assistant director-general who coordinates its work on anti-microbial resistance.
“Without urgent, coordinated action, the world is headed for a post-antibiotic era in which common infections and minor injuries which have been treatable for decades can once again kill.
“Effective antibiotics have been one of the pillars allowing us to live longer, live healthier, and benefit from modern medicine.
“Unless we take significant actions to improve efforts to prevent infections and also change how we produce, prescribe and use antibiotics, the world will lose more and more of these global public health goods and the implications will be devastating.”
The report, “Antimicrobial Resistance: Global Report on Surveillance”, shows that resistance is occurring in many bacteria causing different infections.
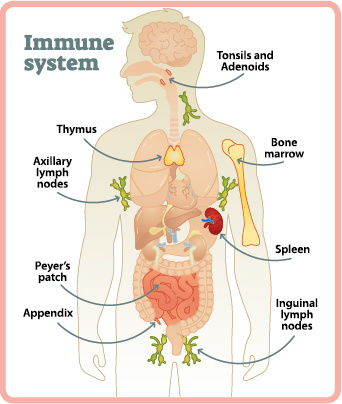
It focuses on antibiotic resistance in seven bacteria responsible for common, serious diseases, such as bloodstream infections (sepsis), diarrhoea, pneumonia, urinary tract infections and gonorrhoea.
What is especially alarming is that the bacteria’s resistance has also breached “last resort” antibiotics, which are the most powerful medicines that doctors resort to when the usual ones do not work.
When patients do not respond to the usual medicines (known as first-line or first-generation medicines), doctors prescribe newer (second line medicines) which also usually also cost more.
When these also don’t work, newer and often more powerful (but sometimes with also more side effects) antibiotics are used, and they are even more expensive.
If these third-line or “last resort” medicines are not available or too costly for the patient, or if they don’t work on a patient because of antibiotic resistance, the patient remains ill or dies if the infection is a serious one.
New antibiotics have been discovered in the past to treat infections when the old ones became useless due to resistance.
But these discoveries dried up in the past 25 years.
The last completely new classes of anti-bacterial drugs were discovered in the 1980s.
Pathogens that are becoming increasingly resistant including to the more powerful antibiotics include E. coli, K. pneumonia, S. aureus, S. pneumonia, salmonelia, shigella and n. gonorrhoeae.
Key findings from the report include:
> Resistance to the treatment of last resort for life-threatening infections caused by a common intestinal bacteria, K. pneumonia — carbapenem antibiotics — has spread worldwide.
K. pneumoniae is a major cause of hospital-acquired infections such as pneumonia, bloodstream infections, infections in newborns and intensive-care unit patients.
In some countries, because of resistance, carbapenem antibiotics would not work in more than half of people treated for K. pneumoniae infections;
> Resistance to one of the most widely used antibacterial medicines for the treatment of urinary tract infections caused by E. coli – fluoroquinolones – is very widespread.
In the 1980s, when these drugs were first introduced, resistance was virtually zero.
In many countries today, this treatment is ineffective in more than half of patients;
> The sexually transmitted disease, gonorrhoea may soon be untreatable unless there are new drugs. Treatment failure to the last resort of treatment for gonorrhoea – third generation cephalosporins – has been confirmed in several countries; and
> Antibiotic resistance causes people to be sick for longer and increases the risk of death.
For example, people with MRSA (methicillin-resistant Staphylococcus aureus) are estimated to be 64% more likely to die than people with a non-resistant form of the infection.
There are many cases of patients being infected by MRSA in hospitals.
The report also gives useful information on the worrisome building up of resistance in four serious diseases — tuberculosis, malaria, HIV and influenza.
A major factor accelerating resistance is in the animal husbandry sector, where there is a liberal use of antibiotics mainly to promote the growth of the animals used for food, for commercial purposes.
This builds up resistance in the bacteria present in the animals.
These resistant germs are passed on to humans who consume the meat.
The report has a small section on the animal-food chain, which has been identified as a major problem.
The European Union has banned the use of antibiotics as growth promoters in animals, but it is still allowed in other countries.
A WHO press release on the report calls for some actions. These include:
> Setting up basic systems in countries to track and monitor the problem;
> Preventing infections from happening in the first place to reduce the need for antibiotics;
> Only prescribing and dispensing antibiotics when they are truly needed, and prescribing and dispensing the right antibiotic(s) to treat the illness;
> Patients using antibiotics only when prescribed by a doctor and completing the full prescription; and
> Developing new diagnostics, antibiotics and other tools to stay ahead of emerging resistance.

Contributed by Global Trends by Martin Khor
Martin Khor is executive director of the South Centre, a research centre of 51 developing countries, based in Geneva. You can e-mail him at director@southcentre.org. The views expressed are entirely his own.
 Related posts:
Related posts: